
.png)
NexHealth Resources
Your hub for patient engagement insights, customer stories, podcasts, software comparisons, events, and webinars.
Popular Resources

NexHealth Spring 2024 Release
Discover new ways to digitize and automate every part of the patient experience

Topics

How to Improve Patient Scheduling and Fill Cancellations
The lack of an efficient process can hinder your practice's schedule optimization, leading to frequent no-shows and cancellations. Here are top-notch strategies to ensure you maximize your practice's schedule.


Patient Scheduling: Tactics To Increase Dental Appointments
Discover the reasons behind more practices adopting online dental appointment scheduling software solutions and which one suits your needs. Learn how these tools can drive appointment bookings, minimize no-shows, and reduce cancellations.


12 Zocdoc Alternatives for Getting New Patients
Looking for a more holistic solution to getting new patients? Click to check out our comprehensive list of the best Zocdoc alternatives.

Case Studies

NADG Turns to NexHealth to Digitize 200+ Practices and 5x New Patient Appointments
See how North American Dental Group consolidated its various software into a single platform with NexHealth — digitizing the patient experience with a 5x increase in the number of new patients


Painless Peach Pain Care syncs athenahealth with NexHealth to digitize the patient experience
Painless Peach Pain Care wanted to deliver a modern patient experience but was stuck taking patient appointments on the phone and relying on paper forms. Using NexHealth with athenahealth made it easy to book patients online and collect patient data: HIPAA consent, medical history, and more. The best part? Every online booking and digital form is synced automatically to athenahealth with the NexHealth Synchronizer.


The Dermatology Specialists Offers 24/7 Booking Accessibility Across 40+ Locations with NexHealth
The Dermatology Specialists are on a mission to revolutionize the dermatology industry by prioritizing patient accessibility. Teaming up with NexHealth, they've crafted a best-in-class digital patient experience.

Podcasts

Key Performance Indicators Every Practice Owner Should Track with Mark Costes
Hear from Mark Costes, CEO of Dental Success Institute, on what important KPIs you should know as a practice owners and strategies to ensure you build a thriving practice.


How to Turn Website Visitors into New Patients with Brad Newman
In this episode of How I Build My Practice, Brad Newman from Dentainment shares strategies to convert your website visitors into paying patients.


The Power of Social Media in Dental Marketing with Jordan Agolli
In this episode of the “How I Grew My Practice” podcast presented by NexHealth, our host Alec Goldman sits down with Jordan Agolli, founder of Force Media, to discuss the power of social media in dental marketing.

Company News

NexHealth Spring 2024 Release
Discover new ways to digitize and automate every part of the patient experience


Introducing the new, easier to use NexHealth
A simpler to use NexHealth to get more done with fewer clicks.


The New NexHealth Waitlist
The NexHealth Waitlist fills canceled appointments in as little as 20 minutes, driving thousands of dollars of revenue for practices per week and increasing patient satisfaction

Compares
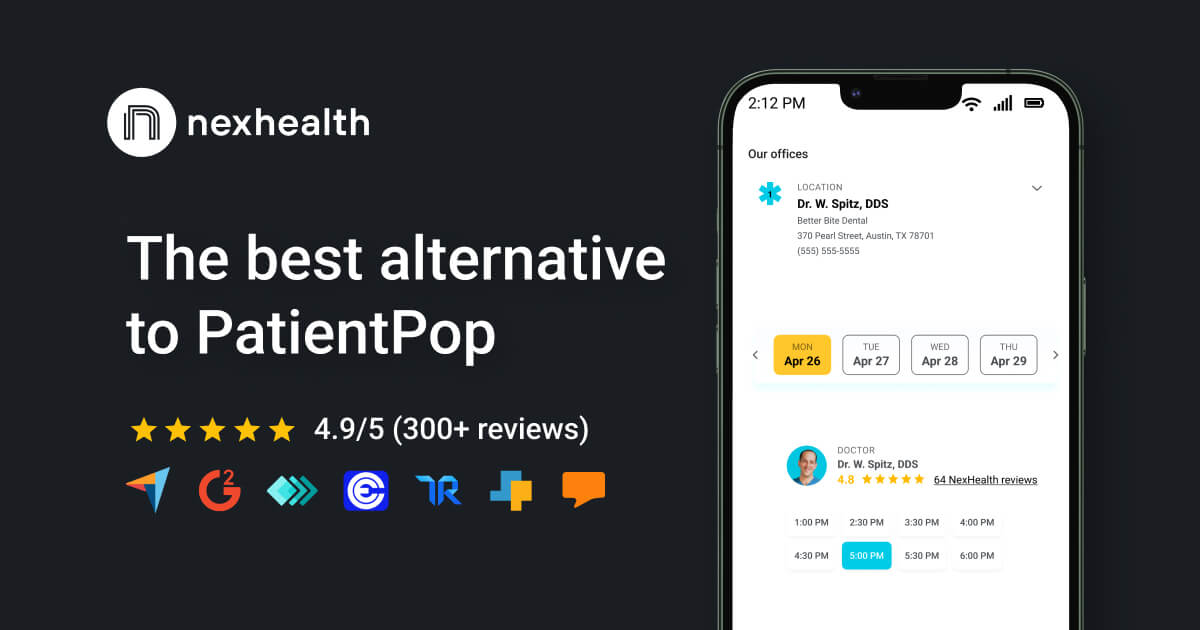
NexHealth Vs. PatientPop | Comparison
Switch to NexHealth for a streamlined patient experience. Our online booking, digital forms, and two-way text features are user-friendly, and our hassle-free integration!


NexHealth vs RevenueWell | Comparison
NexHealth vs. RevenueWell: Choose NexHealth for online booking, digital forms, and two-way text. Enjoy seamless integration with your practice management system.


NexHealth Vs. LocalMed | Comparison
Simplify the patient experience - NexHealth vs. LocalMed. NexHealth offers modern features, seamless integration with practice management. Join now!

Events

Rocky Mountain Dental Conference 2024
Meet us at Rocky Mountain Dental Conference at booth #622 to see a NexHealth demo, receive a complimentary tote, and more!


Yankee Dental Congress 2024
Meet us at Yankee Dental Congress at booth #224 to see how NexHealth can modernize your office, help you get more patients, and save your staff time. We can't wait to see you there!


NexHealth Set to Showcase at the 2023 Gulf Coast Dental Conference
Join NexHealth at the 2023 Gulf Coast Dental Conference, the largest dental meeting on the Gulf Coast, from July 13-14. Discover our revolutionary patient experience platform at Booth #94 and receive exclusive offers, including a complimentary iPad when you sign up at the event. Experience NexHealth's commitment to modernizing dental practices, in-person.

Join thousands of practices who stay up-to-date with the latest practice growth tips and trends.

_BestEstimatedROI_Roi.png)
_BestSupport_QualityOfSupport.png)
















And I've used at least 6 others." - Shaye, Falmouth Dentistry